Neurotransmitter disorders are an expanding group of inherited neurometabolic syndromes that affect children
Neurotransmitters, like dopamine, support a variety of functions in the body, including cognition, emotion, and movement. Dopamine is specifically involved with decision-making, motivation, and motor control.1-3
Within a growing group of genetic conditions referred to broadly as neurotransmitter disorders, many are marked by a disruption in monoamine neurotransmitter synthesis, metabolism, and homeostasis. The disruption in synthesis leads to a range of neurological manifestations in childhood, including1,4:
- Developmental delay
- Motor disorders
- Epilepsy
- Autonomic dysfunction
- Neuropsychiatric features
One neurotransmitter disorder is Aromatic L-amino Acid Decarboxylase (AADC) deficiency, which is a genetic disorder associated with defects in neurotransmitter synthesis that can lead to a manifestation of a broad spectrum of symptoms.
The most common symptoms of this autosomal recessive disorder are5-8:
- Hypotonia
- Developmental delay
- Movement disorders, especially oculogyric crises
Many of the most common symptoms of AADC deficiency can also be attributed to a number of other conditions, resulting in potential misdiagnosis.1,4-6,9-12
Some of these conditions include1,4-6,9-12:
- Cerebral palsy
- Epilepsy
- Juvenile parkinsonism
Unlike juvenile parkinsonism and certain forms of epilepsy, AADC deficiency is not neurodegenerative or multifactorial.2,5,9,13-15
WATCH: What is AADC deficiency?
Phillip Pearl, MD, and Keith Hyland, PhD, give an overview of AADC deficiency
AADC is an enzyme required for biosynthesis of dopamine and serotonin5
In AADC deficiency, mutations in the dopa decarboxylase (DDC) gene result in significant reduction or complete loss of AADC enzyme activity, leading to severe combined deficiency of dopamine, serotonin, norepinephrine, and epinephrine.5,6,16,17
The result of reduced AADC enzyme activity is an increase in L-dopa, 3-OMD, and 5-HTP, and a decrease in the neurotransmitter metabolites HVA and 5-HIAA.5,6,16,17
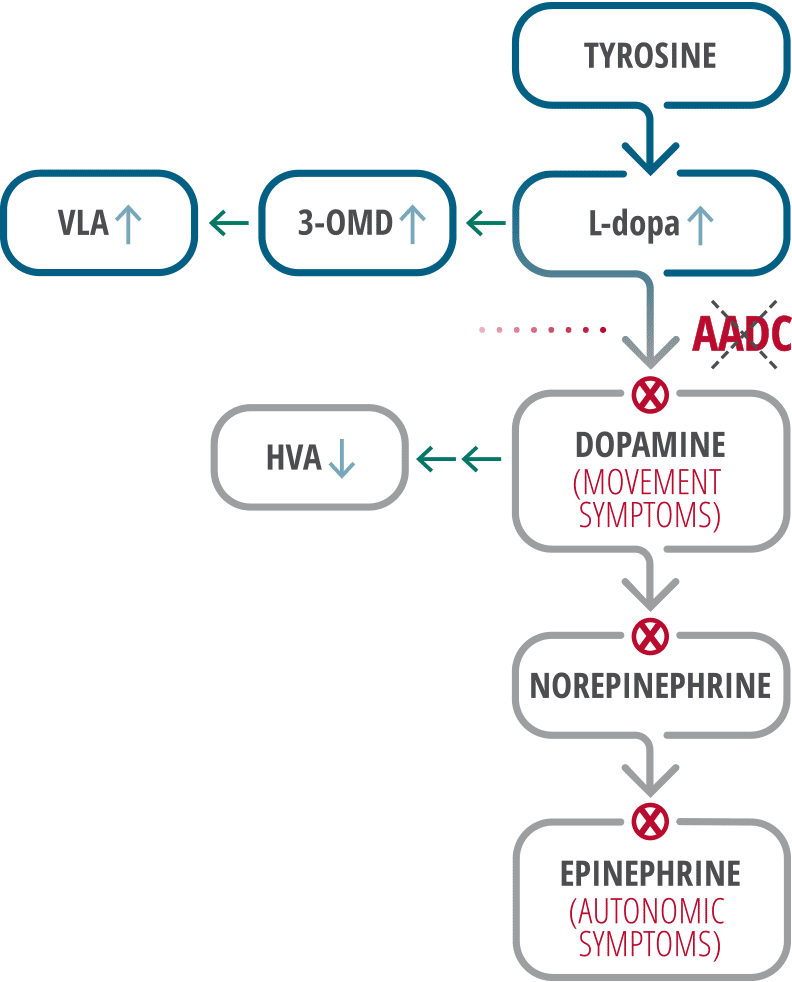
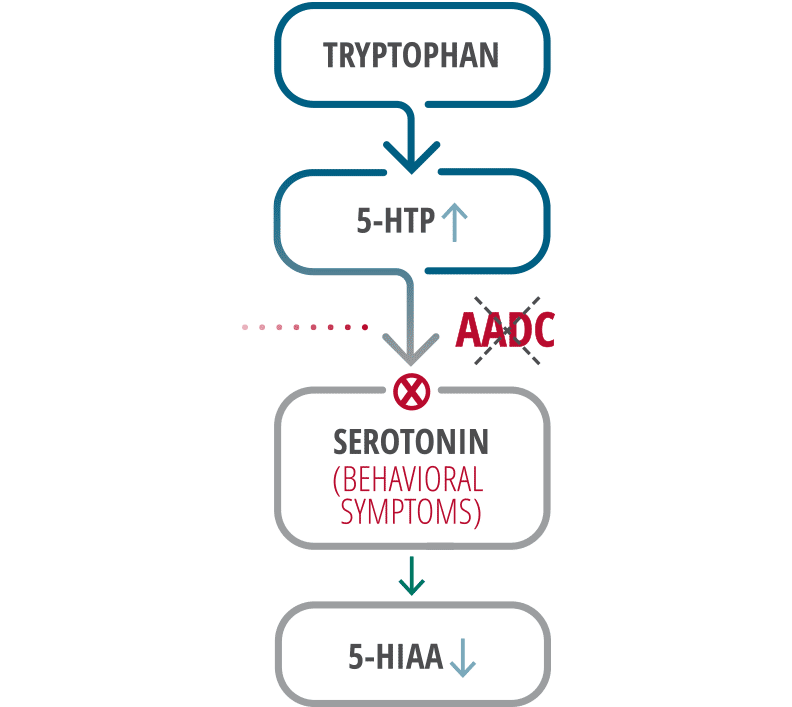
Adapted from Wassenberg 2017.5
3-OMD=3-O-methyldopa; 5-HIAA=5-hydroxyindoleacetic acid; 5-HTP=5-hydroxytryptophan; HVA=homovanillic acid; L-dopa=L-3,4-dihydroxyphenylalanine; VLA=vanillactic acid.
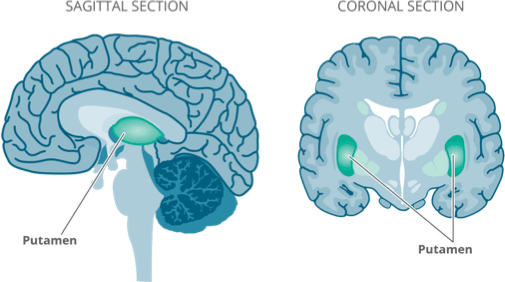
The putamen is a major site of dopamine activity and plays a critical role in motor function18,19
The putamen is part of the dorsal striatum, which plays a key role in corticostriatal connections that determine motor performance. It is a major site of AADC enzyme activity, and, consequently, dopamine activity.2,18,20
As an important site of dopamine signaling, a deficiency of dopamine in the putamen can lead to dopamine depletion and motor dysfunction in patients with AADC deficiency.2,19